Recycling cans and bottles is a good practice. It helps keep the planet clean.
The same is true for recycling within cells in the body. Each cell has a way of cleaning out waste in order to regenerate newer, healthier cells. This ‘cell recycling’ is called autophagy.
Targeting and changing this process has been linked to helping control or diminish certain cancers. Now, University of Cincinnati researchers have shown that completely halting this process in a very aggressive form of breast cancer may improve outcomes for patients one day.
These results are published in the Feb. 8 print edition of the journal Developmental Cell.
“Autophagy is sort of like cell cannibalism,” says corresponding author Jun-Lin Guan, Ph.D., Francis Brunning Professor and Chair of UC’s Department of Cancer Biology. “They eat the nasty components of themselves and come out strong and undamaged; however, we do not want cancer cells doing this to create stronger, healthier versions of themselves. Previous studies found that disabling this process slowed down the growth of another type of breast cancer, but it was unknown whether blocking autophagy could be beneficial for a particularly aggressive type of breast cancer, known as HER2-positive breast cancer.”
This type of breast cancer grows rapidly, and while there are effective treatments, unfortunately, these particular cancer cells find a way to become resistant to therapy, leading to relapse and a higher death rate in patients.
Researchers in this study used animal models to show that blocking autophagy eliminated the development and growth of this type of breast cancer “even to a greater extent than our previous studies in other types of breast cancer,” says Guan, also a member of the UC Cancer Center.
He adds that researchers also uncovered that by blocking this activity, they were able to impact the other activities and mechanisms within the cancer cells completely, changing their roles and reactions.
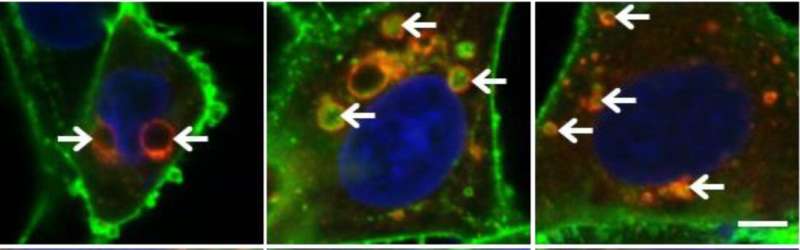
“It altered trafficking patterns of the HER2 protein after it is produced by the cancer cells,” he continues. “Instead of being put in its ‘normal’ location on the cell surface to cause cancer development, it is incorporated into some small fluid-filled pouches, known as vesicles, and secreted out of the tumor cells.”
Guan says these findings are particularly important as they show a completely different way to potentially treat this type of breast cancer and may work as a combination therapy with current treatments to prevent resistance and relapse.
“It would be harder for the cancer cells to develop ways to evade two different ways to be blocked,” he adds. “Future clinical studies will be needed to validate the treatment in human patients. Also, the HER2 protein plays a role in several other cancers including lung, gastric [stomach] and prostate cancers, so future studies will need to examine whether this new mechanism may also be beneficial in treating those cancers as well.
“This study really shows the value of basic research in beating cancer in the future. Breakthroughs, like this one, are sometimes made from curiosity-driven research that result in surprising findings that could one day help people.”
Lead author on the study Mingang Hao, Ph.D., who is a postdoctoral fellow in Guan’s lab, says he was handling two separate cancer research projects at the same time, but this study inspired findings for the other, which also involved vesicles or “bubbles” in cancer spread.
“Cancer research has so many intricate twists and turns, but so much of it can be interconnected, even in tiny ways,” Hao says. “Working with the teams at UC has shown me some really innovative ways to tackle this disease, and I’m able to apply things I’m learning in one lab to research in another, to ultimately help find solutions for this terrible disease.”
Co-author Kevin Turner, MD, a resident in the Department of Surgery at UC, says his work with this science helps him understand more about cancer development and spread to better treat patients.
Source: Read Full Article
