New research may have uncovered a relationship between changes in bacteria in the gut and a rare neurodegenerative disease that primarily affects people in a remote Indigenous community in the Northern Territory.
Researchers at Macquarie University have discovered a possible link between Machado-Joseph disease (MJD) and changes in the bacteria and other microorganisms that populate the gut.
Similar to Huntington’s disease and motor neuron disease (MND), MJD is a debilitating neurodegenerative condition that causes the progressive loss of neurons in parts of the brain and spinal cord.
Neurons are the body’s messenger cells, carrying information to and from the central nervous system, and their loss results in loss of coordination, balance and motor skills, muscle atrophy, and disturbances in vision, speech, and swallowing. It is untreatable and eventually fatal.
Patients begin to feel muscle weakness, then start to stagger as they walk but as the disease progresses, they end up dependent on a wheelchair and in need of high levels of care.
This puts tremendous strain on their families and communities, especially in the remote locations where MJD is most concentrated. It affects people in a number of isolated communities.
Groote Eylandt, 50km off the Northern Territory mainland in the Gulf of Carpentaria, has the highest prevalence of MJD in the world. The tiny island has a population of just 3,000, many of whom are Aboriginal and Torres Strait Islander.
More than 100 people in the community have MJD, and several hundred more have the gene that causes it.
In some families, three generations are battling the disease at once.
The role of gut bacteria
The intestinal tracts of humans and other mammals are naturally home to thousands of species of microbes, including bacteria, fungi, archaea and viruses.
These microscopic organisms make up the gut microbiota, and when they are in balance, they work with our bodies to help maintain metabolic, immune and brain health.
Increasing evidence is showing a relationship between imbalances in the microbiota and metabolic and immune-related conditions including inflammatory bowel disease, diabetes and obesity.
Such imbalances have also been found in people with depression, autism spectrum disorder, and neurodegenerative diseases such as Parkinson’s, Alzheimer’s, Huntington’s and MND.
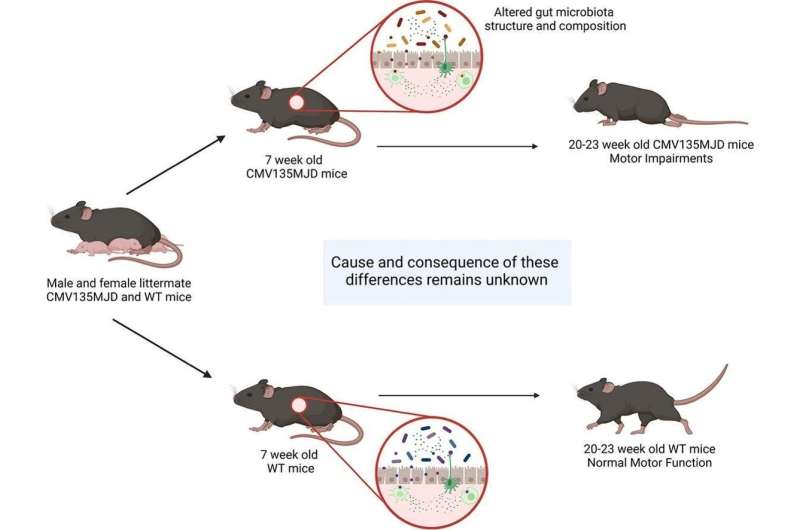
Now for the first time, Associate Professor Angela Laird and her research team have found that mice with MJD also have imbalances in the microbiota, and they have published their findings in a paper in the journal Neurobiology of Disease.
“The gut and the central nervous system have their own communication pathway—the gut-brain axis,” Associate Professor Laird says.
“When the gut microbiota is out of balance, it can have far more wide-ranging effects than only disrupting the digestive system.
“Some people with neurodegenerative diseases such as Parkinson’s disease have gastro-intestinal symptoms early in the disease course.
“From what we know of the gut, it seemed possible that these changes could be caused by an imbalance in the microbiota.”
Looking at mice specially bred to carry the MJD gene, the team was able to observe an increase in the levels of some naturally occurring gut bacteria and a decrease in others well before the onset of any neurological symptoms.
Ph.D. candidate Katherine Robinson says while the genetic cause of MJD has been known since the 1990s, little progress has been made in identifying new treatments that may slow or stop the development of MJD.
“Exploring how changes in the gut microbiota may relate to MJD is an exciting new area to explore that could lead to a treatment breakthrough,” she says.
“MJD is caused by inheriting extra nucleotides—one of the building blocks of human DNA—in a gene called ATXN3 found on chromosome 14.
“The more additional nucleotides inherited in the ATXN3 gene, the earlier symptoms are likely to appear and the faster the disease progresses.
“We also observed this in the mice we studied, and it’s particularly interesting that we saw changes in the gut microbiota well before the onset of the neurological symptoms.
Looking forward to a possible treatment
Lead author Dr. Hasinika Hewawasam Gamage says MJD was linked with substantial shifts in the microbiome, and these changes were different in male and female mice.
“However, there were consistent drops in the abundance of bacterial families Lachnospiraceae, Oscillospiraceae and Rikenellaceae in both males and females well before any of the known symptoms were detected,” she says.
“Interestingly, the extent of the drop in these gut bacteria at the pre-symptomatic stages was indicative of how severe the MJD symptoms were at advanced stages of the disease.
Some of the by-products of microbial metabolism produced in the gut are known to protect the nervous system potentially through encouraging the recycling of dead or damaged cells.
“One of our theories is that the shifts in the gut microbiota may lead to changes in the production of microbial metabolites, such as the short chain fatty acid butyrate and amino acid tryptophan, which could impact this recycling mechanism and preventing the neurons from working properly in MJD.
“We hope that further investigation into how gut microbes influence the progression of MJD may offer options for treatment in the future.
“We are now looking at how the changes in the gut microbes influence the disease progression, with a view to identifying how we could bring about changes in the microbiome to at least help reduce the severity of the symptoms.”
The next step for the team is to begin investigating whether the same changes observed in mice are also found in human patients.
More information:
Hasinika K.A.H. Gamage et al, Machado Joseph disease severity is linked with gut microbiota alterations in transgenic mice, Neurobiology of Disease (2023). DOI: 10.1016/j.nbd.2023.106051
Journal information:
Neurobiology of Disease
Source: Read Full Article