Researchers at NYU College of Dentistry’s Pain Research Center have developed a gene therapy that treats chronic pain by indirectly regulating a specific sodium ion channel, according to a new study published in the Proceedings of the National Academy of Sciences (PNAS).
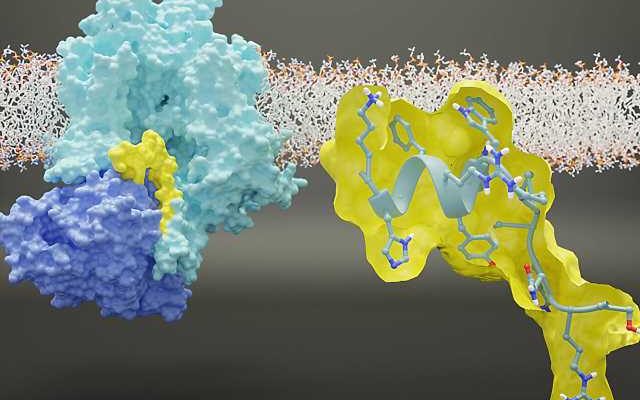
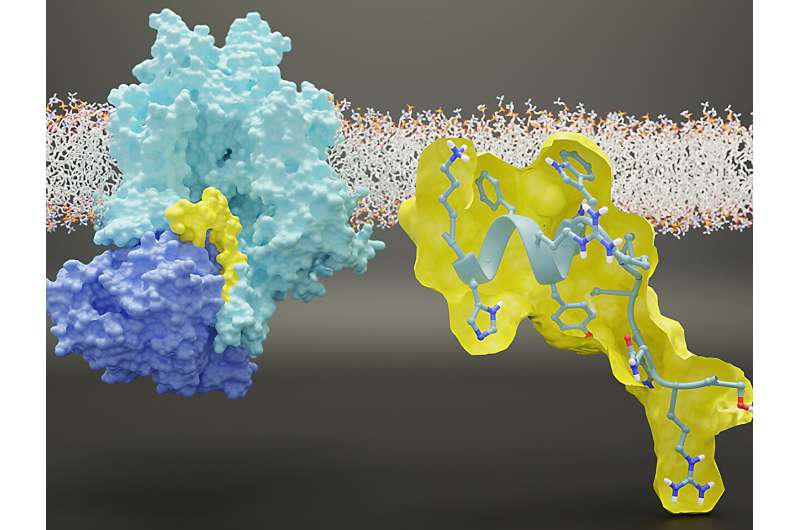
The innovative therapy, tested in cells and animals, is made possible by the discovery of the precise region where a regulatory protein binds to the NaV1.7 sodium ion channel to control its activity.
“Our study represents a major step forward in understanding the underlying biology of the NaV1.7 sodium ion channel, which can be harnessed to provide relief from chronic pain,” said Rajesh Khanna, director of the NYU Pain Research Center and professor of molecular pathobiology at NYU Dentistry.
Chronic pain is a significant public health issue that affects roughly a third of the U.S. population. Scientists are eager to develop pain medications that are more effective and safer alternatives to opioids.
Sodium ion channels play a key role in the generation and transmission of pain, as they are critical for nerve cells, or neurons, communicating with each other. One particular sodium ion channel called NaV1.7 emerged as a promising target for treating pain following the discovery of its importance in people with rare, genetic pain disorders. In some families, a mutation in the gene that encodes for NaV1.7 allows large amounts of sodium to enter cells, causing intense chronic pain. In other families, mutations that block NaV1.7 result in a complete lack of pain.
Scientists have been trying for years to develop pain treatments to selectively block NaV1.7—with little success. Khanna has taken a different approach: rather than blocking NaV1.7, his goal is to indirectly regulate it using a protein called CRMP2.
“CRMP2 ‘talks’ to the sodium ion channel and modulates its activity, allowing more or less sodium into the channel. If you block the conversation between Nav1.7 and CRMP2 by inhibiting the interaction between the two, we can dial down how much sodium comes in. This quiets down the neuron and pain is mitigated,” said Khanna, the PNAS study’s senior author.
Khanna’s lab had previously developed a small molecule that indirectly regulates Nav1.7 expression through targeting CRMP2. The compound has been successful in controlling pain in cells and animal models, and studies are continuing towards its use in humans. But despite the compound’s success, a key question remained: Why does CRMP2 only communicate with the NaV1.7 sodium ion channel, and not the eight other sodium ion channels in the same family?
In their study, the researchers pinpointed a specific region within NaV1.7 where the CRMP2 protein binds to the sodium ion channel in order to regulate its activity. They learned that this region is specific to NaV1.7, as CRMP2 did not readily bind to other sodium ion channels.
“This got us really excited, because if we took out that particular piece of the NaV1.7 channel, the regulation by CRMP2 was lost,” said Khanna.
To limit the communication between CRMP2 and NaV1.7, the researchers created a peptide from the channel that corresponds to the region where CRMP2 binds to NaV1.7. They inserted the peptide into an adeno-associated virus in order to deliver it to neurons and inhibit NaV1.7. Using viruses to transport genetic material to cells is a leading approach in gene therapy, and has led to successful treatments for blood disorders, eye diseases, and other rare conditions.
The engineered virus was given to mice experiencing pain, including sensitivity to touch, heat, or cold, as well as peripheral neuropathy that results from chemotherapy. After a week to 10 days, the researchers assessed the animals and found that their pain was reversed.
“We found a way to take an engineered virus—containing a small piece of genetic material from a protein that all of us have—and infect neurons to effectively treat pain,” said Khanna. “We are at the precipice of a major moment in gene therapy, and this new application in chronic pain is only the latest example.”
The researchers replicated their findings inhibiting NaV1.7 function across multiple species, including rodents and the cells of primates and humans. While more studies are needed, this is a promising sign that their approach will translate into a treatment for humans.
“There is a significant need for new pain treatments, including for cancer patients with chemotherapy-induced neuropathy. Our long-term goal is to develop a gene therapy that patients could receive to better treat these painful conditions and improve their quality of life,” said Khanna.
In addition to Khanna, study authors include Kimberly Gomez, Paz Duran, Santiago Loya, Cheng Tang, Aida Calderon- Rivera, May Khanna, and Samantha Perez-Miller of NYU Dentistry; Harrison J. Stratton, Liberty François-Moutal, Cynthia L. Madura, Shizhen Luo, Dongzhi Ran, and Lisa Boinon of the University of Arizona; Bryan McKiver, Edward Choi, and M. Imad Damaj of Virginia Commonwealth University; and Aubin Moutal of St. Louis University.
More information:
Kimberly Gomez et al, Identification and targeting of a unique Na V 1.7 domain driving chronic pain, Proceedings of the National Academy of Sciences (2023). DOI: 10.1073/pnas.2217800120
Journal information:
Proceedings of the National Academy of Sciences
Source: Read Full Article