Lung cancer patients with moderate to severe depression are two to three times more likely to have inflammation levels that predict poor survival rates, a new study found.
The results may help explain why a substantial portion of lung cancer patients fail to respond to new immunotherapy and targeted treatments that have led to significantly longer survival for many people with the disease.
“These patients with high levels of depression are at much higher risk for poor outcomes,” said Barbara Andersen, one of the lead authors of the study and professor of psychology at The Ohio State University.
“Depression levels may be as important or even more important than other factors that have been associated with how people fare with lung cancer.”
The study was published online recently in the journal PLOS ONE.
Andersen and colleagues at Ohio State’s College of Medicine and The Ohio State University Comprehensive Cancer Center—Arthur G. James Cancer Hospital and Richard J. Solove Research Institute studied 186 patients who were newly diagnosed with advanced lung cancer (Stage IV). They were interested in how depression levels were related to systemic inflammation ratio (SIR) biomarker levels at diagnosis.
SIRs include three biomarkers associated with inflammation in the body. Higher inflammation is more dangerous and linked to lower survival rates.
All participants also completed a depression measure. The results showed that a large proportion of patients—35%—had moderate to severe depressive symptoms.
“Of all cancer patients, those with lung cancer are among those with the highest rates of depression, which makes the findings of our study even more concerning,” Andersen said.
Results showed an association between higher depression scores and higher inflammation scores, but the key finding was that patients with the highest depression levels were driving the relationship, Andersen said.
For example, take the platelet-to-lymphocyte ratio, one of the biomarkers in the study. For those with no or mild depression symptoms, 56% of patients were above the cutoff for dangerous levels of inflammation, versus 42% who were below.
But for those with high depression levels, 77% were above the cutoff for high levels of inflammation and only 23% were below.
“It was patients with high depression levels who had strikingly higher inflammation levels, and that is what really drove the correlation we saw,” she said.
These highly depressed patients were 1.3 to 3 times more likely to have high inflammation levels, even after controlling for other factors related to inflammation biomarker levels, including demographics and smoking status.
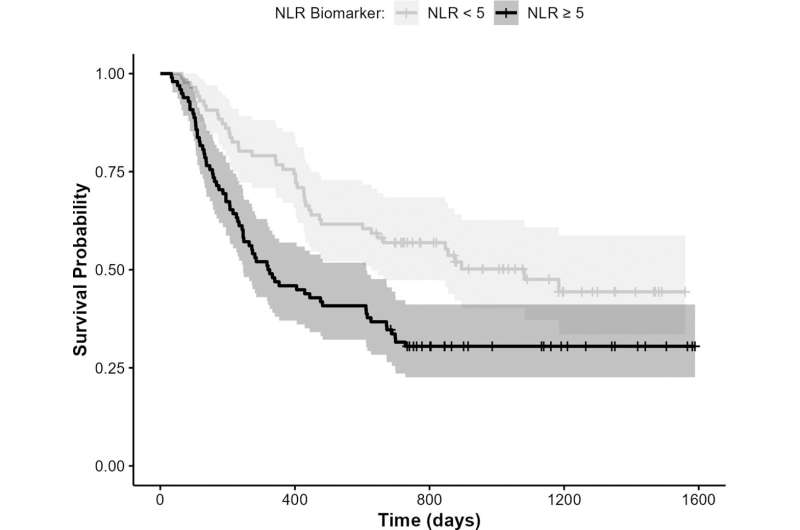
And analyses had shown that the baseline levels of all three biomarkers predicted overall survival. Specifically, patients with elevated neutrophil-to-lymphocyte ratios (one of the inflammatory biomarkers) were approximately twice as likely to die at any time point in the next two years compared to those with a lower inflammation ratio.
Andersen noted that this study measured the link between depression and inflammation when patients were first diagnosed, and as yet untreated.
But in a previous study by Andersen and her colleagues, they controlled for depression levels at diagnosis and found that the trajectory of continuing depression symptoms thereafter predicted survival. This was the first examination of the survival risk posed when depressive symptoms continue through treatment and thereafter.
The accumulating data suggest the importance of measuring and treating depression in patients with lung cancer, Andersen said.
She noted that there were more patients in this study with high depression/elevated inflammation than those having other indicators associated with poor survival in cancer patients: high school or lower education, overweight status, and a poor score on a test of ability to perform everyday activities.
Some doctors may think it is normal for cancer patients to be depressed, but that’s not true, she said.
“It is normal to be upset, sad and anxious about a cancer diagnosis, but it is not normal to have major depression,” Andersen said.
“Depression should not be discounted. This study shows the strong link between depression and inflammation, with both related to poor outcomes.”
More information:
Barbara L. Andersen et al, Depression in association with neutrophil-to-lymphocyte, platelet-to-lymphocyte, and advanced lung cancer inflammation index biomarkers predicting lung cancer survival, PLOS ONE (2023). DOI: 10.1371/journal.pone.0282206
Journal information:
PLoS ONE
Source: Read Full Article