MADRID — The positive effect of the bispecific fusion protein tebentafusp on the overall survival of patients with uveal melanoma in the IMCgp100-202 study lasted through at least 36 months of follow-up. After 3 years, 27% of patients in the tebentafusp group had survived, compared with 18% in the control group.
“Tebentafusp is the only therapy to demonstrate a beneficial effect on the long-term survival of patients with HLA-A*02:01-positive uveal melanoma,” said Sophie Piperno-Neumann, MD, PhD, medical oncologist at the Institut Curie, Paris, at the European Society for Medical Oncology (ESMO) Annual Congress 2023. The 3-year results of the IMCgp100-102 study were published at the same time in The New England Journal of Medicine. Most of the adverse events associated with tebentafusp occurred in the first month of treatment, and their frequency and severity decreased as the study continued.
One discussant, Omid Hamid, MD, an oncologist at the Cedars-Sinai Cancer Center in Los Angeles, indicated that similar results have been achieved with tebentafusp against metastatic cutaneous melanoma and that the substance could be effective against various tumors. He believes that combination therapies will be promising.
Poor Prognosis
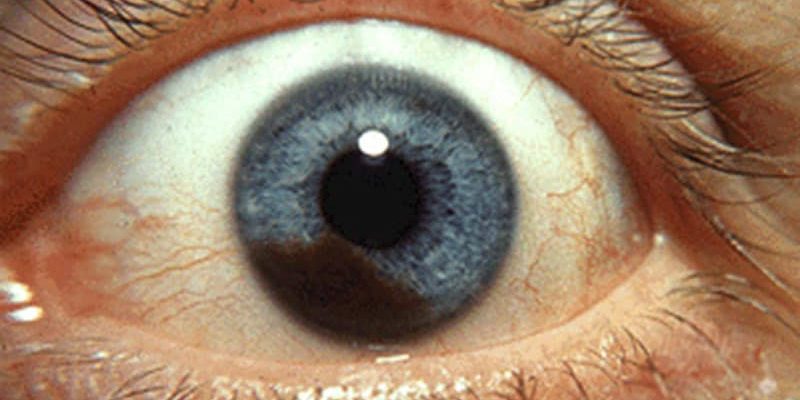
Uveal melanomata account for up to 5% of all melanomata. They metastasize in approximately half of affected patients, predominantly to the liver, lungs, bones, and skin. After metastasis, the prognosis is poor. The median overall survival rate has historically been 1 year. Despite revolutionizing the treatment of cutaneous melanomata, immune checkpoint inhibitors have largely been ineffective against uveal melanoma.
Tebentafusp is the first T-cell receptor, bispecific fusion protein (specific for glycoprotein 100 [gp100] and CD3) that triggers T cells to target gp100-positive melanoma cells. Tebentafusp (Kimmtrak) is the only approved systemic therapy for adult HLA-A*02:01-positive patients with unresectable or metastatic uveal melanoma.
The IMCgp-100-202 Study
In the primary analysis of the phase 3 IMCgp100-202 study, which included 378 previously untreated patients with metastatic uveal melanoma, the tebentafusp treatment significantly improved overall survival (OS), compared with the control therapy. According to the investigator’s choice, the control therapy was monotherapy with pembrolizumab, ipilimumab, or dacarbazine. In the open-label, randomized study, 252 patients received tebentafusp, and 126 patients received the comparator therapy — mostly pembrolizumab.
The overall survival after 1 year was 73% in the tebentafusp group and 59% in the control group (hazard ratio [HR], 0.51; P < .001). The progression-free survival was also significantly better in the tebentafusp group than in the control group (31% vs 19% after 6 months [HR, 0.73; P = .01]). The HR for death was 0.51 (P < .001); 73% and 59% of the patients, respectively, survived 1 year.
Durable Effect
The patients were followed for at least 36 months. The positive effect of tebentafusp on OS continued to last. The median survival of the patients was 21.6 months with tebentafusp, compared with 16.9 months in the comparator group (HR, 0.68). The 3-year OS was 27% in the tebentafusp group and 18% in the control group. With tebentafusp, a response rate of 11% and a disease control rate of 46% were achieved. The corresponding rates for the comparator therapy were 5% and 27%, respectively. The median response lasted for 11.1 or 9.7 months, respectively.
The ctDNA level was used as a prognosis parameter: patients in whom no ctDNA was initially detectable survived for longer than patients with elevated ctDNA levels. Patients in whom ctDNA was no longer detectable at week 9 also survived longer than those with ongoing positive ctDNA evidence.
The OS for the 99 patients in whom the ctDNA level decreased by at least 50% was longer than for the 24 patients in whom it decreased by less than 50%, did not change, or increased. “The role of ctDNA as an indicator for the initial benefit, which is overlooked by RECIST, cannot be overstated here,” said Hamid.
Therapy-related adverse events mainly occurred at the start of treatment, after which they decreased. Most adverse events commonly associated with tebentafusp were skin rash, fever, itching, and a drop in blood pressure. Side effects of a severity of ≥3 developed in 47% of patients. During the 3-year follow-up, no new adverse events were observed.
This article was translated from the Medscape German edition.
Source: Read Full Article