
Crohn’s disease affects four million people worldwide. The condition causes debilitating symptoms such as chronic fatigue, diarrhea, abdominal pain, weight loss and malnutrition. Once symptoms develop, Crohn’s is a lifelong condition—and while there are ways to manage symptoms during flare-ups, there’s currently no cure.
The exact causes of Crohn’s disease are unknown and are probably due to a number of complex and overlapping factors—such as genetics, environmental cues (such as smoking) and an immune system that’s overactive in the gut. Research has also shown that the gut microbiome plays a crucial role in the disease.
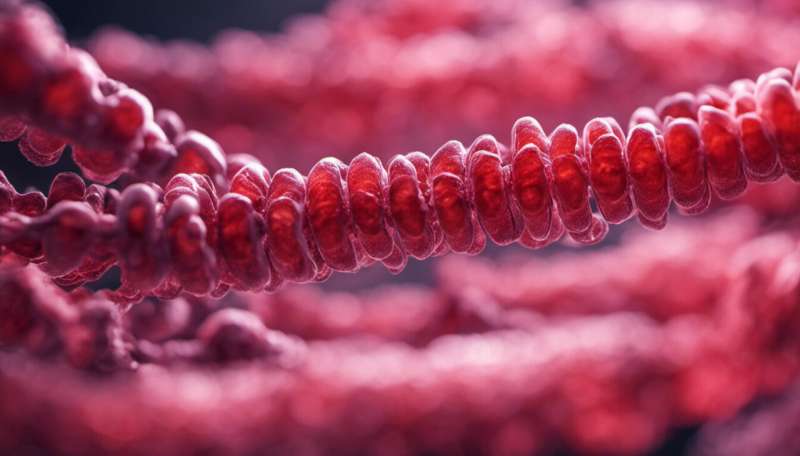
The gut microbiome is a collection of trillions of bacteria, viruses and fungi. These microbes are present from birth and play a crucial role in ensuring the gut cells and our intestines function as they should. The bacteria in our gut also help our immune cells function as they should, ultimately ensuring it is effective.
Many studies show that people with Crohn’s disease have a less diverse community of gut bacteria. They also have higher levels of certain types of bacteria that can trigger gut inflammation.
But it isn’t only the gut’s bacteria that show signs of dysfunction in people with Crohn’s disease. Rather unexpectedly, research also shows that the bacteria in the mouth might also be important in this inflammatory condition.
Mouth microbiome
When we’re in the womb, our gut is sterile. But our gut microbiome begins to develop the moment we’re born—first after coming in contact with vaginal bacteria during birth, then from other maternal sources such as breast milk and skin, as well as our environment.
By the time we’re adults our gut becomes a thriving community of trillions of bacteria which, by some estimates, outnumber our cells by 10:1.
Most of the bacteria that make it to our guts had to travel through our mouths first. As such, our mouth contains the second highest number of bacteria after the gut. And, we swallow these millions of bacteria daily in our saliva.
The oral microbiome is complex. Each part of our mouth—whether it’s the tongue, cheek or our saliva—is composed of different microbes depending on factors such as pH level and oxygen levels. These communities of microbes can then form complex structures called biofilms, where bacteria organize themselves on mouth surfaces (dental plaque is one example). The bacteria then interact with each other and our immune cells to create a harmonious state of health.
There are a couple of reasons why researchers think the oral microbiome might play a role in Crohn’s disease.
First, studies indicate that people with Crohn’s disease have different bacteria in their mouths compared to those without the condition. This could suggest that certain species of bacteria present in the mouth may play a role in Crohn’s disease.
Second, a few species of bacteria commonly found in higher abundances in the intestine of people with Crohn’s disease compared to healthy people are also present in the mouth. This is perhaps unsurprising, given the entry route of bacteria into the lower gut is generally via the mouth. In fact, it’s not uncommon for people with Crohn’s disease to develop ulcers in the mouth, alongside those commonly seen in the gut.
Research in humans also suggests that one oral bacterium in particular, called Veillonella parvula, is abundant in the guts of people with Crohn’s disease. This bacterium is associated with diseases such as periodontitis and even meningitis. It’s typically found in the oral microbiome, but one notable study has shown it has developed a way to live in the lower gut.
If other bacterial culprits of Crohn’s found in the gut are also found in the mouth, this might allow researchers to develop better tests that only need a saliva sample to diagnose the disease. This would be much easier than needing patients to provide a stool or gut tissue sample.
Researchers will also need to investigate whether the oral microbiome may cause Crohn’s. Research in mice suggests that inflammation (which happens when the immune system is triggered by a pathogen) makes it easier for certain types of bacteria to grow—leading to even greater inflammation and an over-activation of immune cells. If the same is true of the oral bacteria linked to Crohn’s disease, it could suggest that bacterial overgrowth and inflammation in the mouth is a possible root cause of Crohn’s.
Other diseases
Crohn’s is not the only disease in which certain mouth bacteria are implicated.
For instance, researchers have shown that two toxic chemicals produced by the oral bacteria Porphyromonas gingivalis (which is involved in gum disease) were found in more than 96% of participants in brain regions associated with memory. Significantly, these toxic chemicals feed on human cells.
In breast cancer, the oral bacteria Fusobacterium nucleatum has been linked with accelerated tumor growth and the spread of cancer cells. Many studies have also shown that the same bacterium is often found in colorectal cancer tissues.
Additionally, there has been a long-held idea that oral bacteria may have a substantial impact on cardiovascular disease, where microbes may leak into the bloodstream and take residence in heart plaques, leading to inflammation—and thus a higher likelihood of rupture or blood vessel blockage.
Although the oral microbiome has been associated with the development and progression of Crohn’s disease, research has not fully worked out the exact way by which bacteria may move from the mouth to parts of the gut. And although there’s plenty of data from mouse studies, more research showing this link in humans is needed.
Better understanding how the oral bacteria are involved in Crohn’s disease—and which species may be implicated—will help develop better diagnostics and treatments, not only for Crohn’s disease but many other conditions as well.
Provided by
The Conversation
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Source: Read Full Article
