Are all fats equal in heart disease risk? New veteran study suggests not
In a recent study published in The American Journal of Clinical Nutrition, a group of researchers in the United States investigated the impact of different types and amounts of dietary fatty acids on the incidence of atherosclerotic cardiovascular diseases (ASCVDs) in a large cohort of United States (U.S.) veterans.
 Study: Association of dietary fatty acids with the risk of atherosclerotic cardiovascular disease in a prospective cohort of United States veterans. Image Credit: Corona Borealis Studio / Shutterstock
Study: Association of dietary fatty acids with the risk of atherosclerotic cardiovascular disease in a prospective cohort of United States veterans. Image Credit: Corona Borealis Studio / Shutterstock
Background
ASCVDs lead global adult deaths, with diet playing a crucial role. Current guidelines generalize fat intake, categorizing fats (saturated, trans, cis, and conjugated) without considering individual fatty acids (FAs) unique effects. This oversimplification ignores varying health impacts, evidenced by recent research challenging traditional views on dietary fats and heart health. Thus, understanding individual FAs' specific influences on ASCVD is critical, necessitating further research for refined dietary recommendations and policies.
About the study
The Million Veteran Program (MVP), initiated in January 2011, had enrolled 702,740 veterans by November 2018. This study focused on the 352,874 individuals who completed the MVP Lifestyle Survey, reporting on their habitual dietary intake. The study excluded participants with pre-existing conditions like ASCVD or cancer, leading to a final cohort of 158,198 for analysis. The median follow-up period was 3.4 years, with all procedures complying with Department of Veterans Affairs policies.
Dietary intake was assessed using a validated Food Frequency Questionnaire (FFQ), which surveyed participants on their average consumption frequency of 61 different foods over the previous year. Intakes of 27 commonly consumed fatty acids and nutrients were then calculated using the Harvard University Food Composition Table. For this study, fat intake was expressed as a percentage of total daily caloric intake.
Various covariates were assessed, including demographics, lifestyle, and medical history, gathered from the Lifestyle Surveys or the Corporate Data Warehouse and MVP Baseline. Body Mass Index (BMI) was calculated, and electronic health records were used for additional data like statin use. ASCVD outcomes were determined based on the International Classification of Diseases (ICD)9 and ICD10 codes from Veterans Affairs electronic health records, with fatalities from the National Death Index used for censoring.
The study outlined a precise chemical analysis at the Harvard T.H. Chan School of Public Health to measure fatty acid content in oils and fats, using extraction, multiple chemical steps, and GC-FID analysis.
The study employed Cox proportional hazard models for statistical analysis, calculating person-time from FFQ completion to the initial ASCVD incident, coronary procedures, or censoring. Participants were divided into quintiles based on the percentage of calories from various fats. Adjustments were made for factors like demographics, health, lifestyle, and medication. The analysis, conducted via SAS Enterprise Guide 8.3, also examined the effects of substituting fats or macronutrients on ASCVD risk, setting statistical significance at a P value under 0.05 and applying the Bonferroni correction for multiple comparisons.
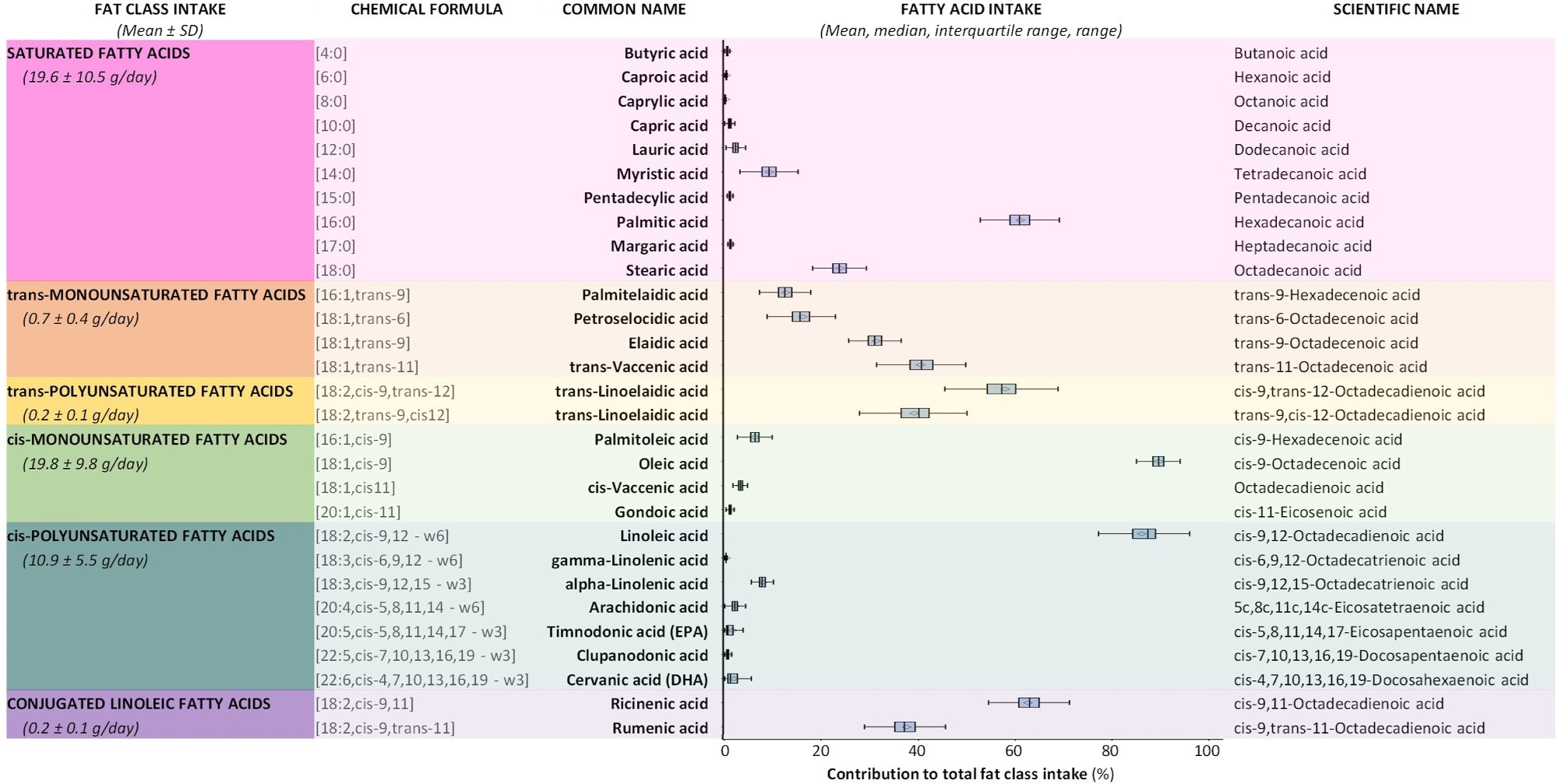 Baseline estimated daily intake of fat classes (represented as absolute intake in grams per day) and individual FAs (represented as percentage contribution to total fat class intake) n = 158,198.
Baseline estimated daily intake of fat classes (represented as absolute intake in grams per day) and individual FAs (represented as percentage contribution to total fat class intake) n = 158,198.
Study results
The present study delves into the dietary patterns of 158,198 U.S. veterans with an average age of 61, focusing on their fat consumption in relation to ASCVD risks. The participants, on average, derived 32% of their total daily calories from fats. Throughout the follow-up, 11,771 ASCVD events were noted, predominantly ischemic heart disease (IHD), followed by ischemic cerebrovascular disease (ICVD) and peripheral arterial disease (PAD).
Significant attention was paid to the intake of saturated fatty acids (FAs), notably palmitic acid, which constituted over half of the total saturated fats consumed. Higher saturated fat intake was observed to correlate with increased ASCVD risk, a consistent finding even after accounting for BMI. Interestingly, replacing saturated fats with cis-polyunsaturated fats reduced ASCVD risk. However, when specific ASCVD components were considered, higher saturated fat intake was linked with PAD but not IHD or ICVD.
The study delved deeper into the effects of individual saturated FAs, revealing that while a higher intake of butyric acid, a short-chain FA, was linked to a lower ASCVD risk, increased consumption of margaric acid, present in dairy and beef fats was associated with a heightened risk of the same. Palmitic acid also showed an elevated ASCVD risk association, which, however, weakened after BMI adjustment.
The analysis extended to trans-unsaturated FAs, revealing that higher consumption levels were connected with a more significant likelihood of experiencing ASCVD events. This association persisted for trans-monounsaturated fats even after BMI inclusion in the models, particularly increasing risks for IHD and PAD.
When considering cis-unsaturated FAs, the main focus was on oleic acid, which comprised the majority of daily cis-monounsaturated fat intake. These fats, however, showed no significant association with ASCVD risk. On the other hand, higher consumption of certain fats like palmitoleic acid and cis-vaccenic acid corresponded to increased ASCVD risk. Notably, participants with higher cis-polyunsaturated fat intake, especially linoleic acid, showed a lower likelihood of ASCVD events.
Finally, the study found that the majority of conjugated linoleic acid intake came from ricinenic FA, and those in the highest consumption quintile faced a greater likelihood of ASCVD events, a risk particularly pronounced for IHD and PAD. The comprehensive analysis underscores the nuanced impacts of various fatty acids on cardiovascular health, highlighting the complexity of dietary influences on disease risk and the potential health benefits of selecting healthier fats.
- Kerry L. Ivey, Xuan-Mai T. Nguyen, Ruifeng Li, et al. Association of dietary fatty acids with the risk of atherosclerotic cardiovascular disease in a prospective cohort of United States veterans, The American Journal of Clinical Nutrition,2023, DOI- https://doi.org/10.1016/j.ajcnut.2023.07.014, https://www.sciencedirect.com/science/article/pii/S0002916523660587
Posted in: Men's Health News | Medical Research News | Medical Condition News | Women's Health News
Tags: Body Mass Index, Cancer, Cardiovascular Disease, Cerebrovascular Disease, Chemical Analysis, Conjugated Linoleic Acid, Diet, Fatty Acids, Food, Frequency, Heart, Heart Disease, International Classification of Diseases, Ischemic Heart Disease, Linoleic Acid, Nutrients, Nutrition, Peripheral Arterial Disease, Public Health, Research, Saturated Fats, Statin, Veterans Affairs

Written by
Vijay Kumar Malesu
Vijay holds a Ph.D. in Biotechnology and possesses a deep passion for microbiology. His academic journey has allowed him to delve deeper into understanding the intricate world of microorganisms. Through his research and studies, he has gained expertise in various aspects of microbiology, which includes microbial genetics, microbial physiology, and microbial ecology. Vijay has six years of scientific research experience at renowned research institutes such as the Indian Council for Agricultural Research and KIIT University. He has worked on diverse projects in microbiology, biopolymers, and drug delivery. His contributions to these areas have provided him with a comprehensive understanding of the subject matter and the ability to tackle complex research challenges.