UC San Diego Health and the Altman Clinical and Translational Research Institute, part of UC San Diego School of Medicine, will be sites for an accelerated national clinical trial to assess the efficacy and immunogenicity of a vaccine intended to protect against SARS-CoV-2, the novel coronavirus that causes COVID-19.
The trial, sponsored by the National Institutes of Health’s (NIH) newly formed COVID-19 Prevention Network (CoVPN), is based upon a vaccine prototype developed by Moderna, a pharmaceutical company located in Massachusetts. The trial is slated to begin July 27.
“Our country and the world are facing an unprecedented pandemic that has already killed more than 600,000 people worldwide,” said Stephen Spector, MD, Distinguished Professor of Pediatrics, Division of Pediatric Infectious Diseases in the UC San Diego School of Medicine and principal investigator for the UC San Diego arm of the vaccine trial.
“A vaccine is desperately needed to help control the epidemic. We are excited that UC San Diego will be able to offer the San Diego community the opportunity to participate in a Phase III vaccine trial that, if successful, has the potential to change the course of the epidemic.”
Historically, new vaccines require years of research and development, progressing sequentially through a series of phases, beginning with a first basic assessment for safety to ensure the experimental drug causes no serious harm. Subsequent Phase II and Phase III trials are intended to establish proof of concept, appropriate dosage, scope of side effects and overall effectiveness based upon a sufficiently large sample size.
Early data from the Phase I clinical trial of the Moderna vaccine, which began in mid-March, was sufficiently encouraging that the NIH, the National Institute for Allergy and Infectious Diseases (NIAID) and Moderna have expedited the process, launching the Phase III trial.
Moderna published its first trial data in The New England Journal of Medicine on July 14, 2020. Researchers reported that participants who received the two-dose vaccine produced more neutralizing antibodies to the novel coronavirus than have been seen in most patients who have recovered from COVID-19. Neutralizing antibodies are part of the body’s adaptive immune system. By interfering with how pathogens, such as viruses, bacteria and microbial toxins, interact with host cells, the antibodies can render pathogens non-infectious.
The Phase I trial cohort was split between three groups receiving 25-microgram, 100-microgram or 250-microgram injections in the arm, spaced 28 days apart, with resulting antibody levels higher with higher dosages. The vaccine was generally well tolerated. No serious side effects were reported, but more than half of participants described temporary fatigue, chills, headache and muscle pain. The largest dose produced more serious reactions and will not be used in the Phase III study, which will test only the 100-microgram dose.
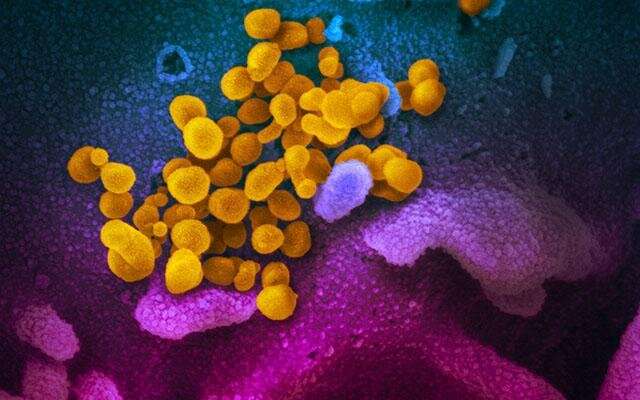
The Moderna vaccine is designed to elicit an immune response against the coronavirus based on the virus’ own mRNA sequence or genetic instructions that guide its replication inside host cells. The vaccine stimulates host cells to produce antibodies against the pathogen. mRNA vaccines are faster to develop than traditional DNA-based vaccines, but none have yet been approved for human use.
The Phase III trial, with the Fred Hutchinson Cancer Research Center in Seattle as lead coordinating institution for the CoVPN, will recruit up to 30,000 participants at multiple sites across the nation. At UC San Diego, the trial will be conducted through the Mother, Child and Adolescent Program (MCAP), which has extensive experience in evaluation of novel vaccines. Spector is director.
UC San Diego is one of three participating trial sites in the region, and expects to enroll approximately 500 subjects.
Participation Protocol
The study trial will be randomized, observer-blind and placebo-controlled—the gold standard for clinical trials—with a primary objective to demonstrate efficacy of the vaccine to prevent COVID-19 and a secondary goal to assess whether it can prevent severe symptoms and death associated with COVID-19.
Participants must be 18 years or older with no known history of SARS-CoV-2 infection. The trial will give preference to participants who live in locations or under circumstances that put them at appreciable risk. For example:
- persons working in essential jobs, such as first responders, health care or grocery stores
- persons living in densely populated residential environments or living/working in congregated facilities, such as nursing homes
- persons belonging to demographic groups disproportionately impacted by the pandemic, such as older persons, persons with underlying health conditions or some racial/ethnic groups, such as African Americans, Latinx and Native American populations
Participants will be randomly and evenly assigned to receive either injections of the test vaccine or a placebo. Every person in both cohorts will receive two injections (vaccine or placebo) 28 days apart, and will be monitored through regular clinic visits and testing over at least two years to see who becomes infected and the outcome.
Full enrollment of vaccinated participants is projected within two months, with an expectation of actionable results by end of year, based upon predetermined, statistically sound endpoints, such as number of infections that occur or were prevented.
Simultaneous to vaccine testing, officials plan to begin actually producing the test vaccine in large amounts so that, if proven effective, there would be significant numbers of doses available by the end of 2020 or early 2021. Typically, vaccines are not produced in great quantities until clinical testing is completed and the drug has been formally approved for wide-scale use. Conducting testing and production at the same time is called “developing at risk,” a costly approach that pays off only if the vaccine proves to be effective.
Source: Read Full Article
