The Omicron variant of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was first reported in November 2021 and rapidly rose to dominance in most parts of the world. This original sublineage is the BA.1 variant and showed the ability to evade most neutralizing antibodies elicited by the earlier variants or by vaccines and monoclonal antibodies (mAbs). A new research paper published as an early release manuscript in the Nature Medicine journal compares the sensitivity of this strain as well as the earlier Delta and the newer BA.2 to therapeutic mAbs.
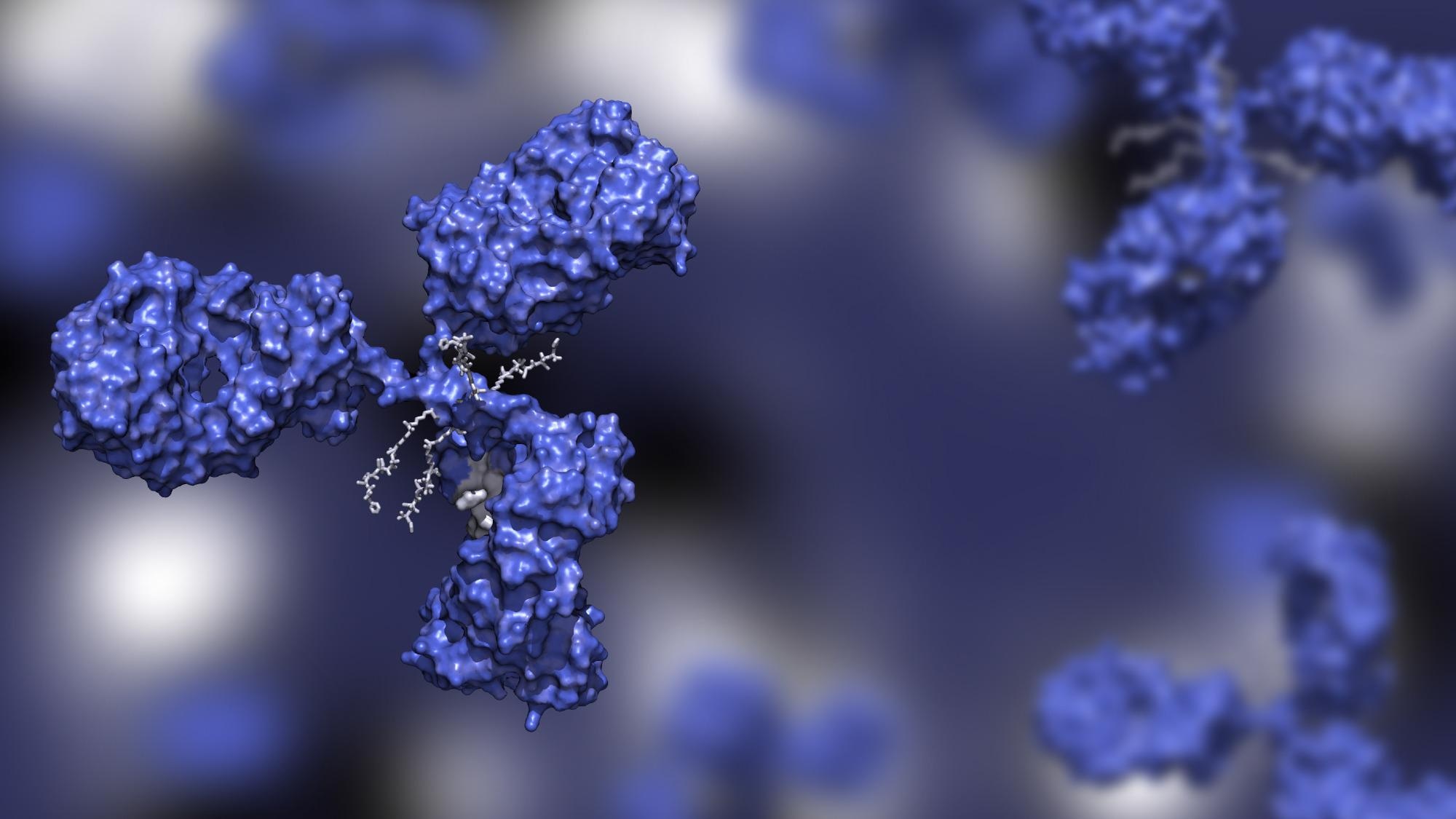 Study: Serum neutralization of SARS-CoV-2 Omicron sublineages BA.1 and BA.2 in patients receiving monoclonal antibodies. Image Credit: Huen Structure Bio
Study: Serum neutralization of SARS-CoV-2 Omicron sublineages BA.1 and BA.2 in patients receiving monoclonal antibodies. Image Credit: Huen Structure Bio
Introduction
Currently, the BA.2 strain is on the increase worldwide, indicating its higher transmissibility and fitness over BA.1. The difference between the two is in 20 spike mutations. The BA.2 has 28 differences in the spike protein compared to the earlier Delta VOC, 18 being common to BA.1. Many of these are in the N-terminal domain (NTD). Both form syncytia of similar size.
BA.2 is less effectively neutralized by vaccine recipient sera than the wildtype and earlier variants of concern (VOCs) and is less sensitive to a number of neutralizing mAbs.
Most neutralizing antibodies target the receptor-binding domain (RBD) of the viral spike protein. Several combinations of such mAbs are used therapeutically, such as Ronapreve (Imdevimab and Etesivimab) from Regeneron and Evusheld (Cilgavimab and Tixagevimab) from AstraZeneca.
Earlier research showed that the risk of infection was reduced to an eighth with Ronapreve, while symptomatic disease was reduced to the same degree with Evusheld. Both have been approved for emergency use in several countries as pre-exposure prophylaxis (PrEP).
A significant drawback is the failure of these cocktails to neutralize BA.1 completely, with the 50% inhibitory concentration (IC50) of Evusheld increasing by 11-180-fold compared to the wildtype. At the same time, Ronapreve showed no neutralization at all. While this led to the use of the former for PrEP in individuals with weakened immunity, other scientists explored the feasibility of using the pan-coronavirus mAb Sotrovimab in high-risk individuals.
The current study compares the neutralization of BA.1 and BA.2 by nine therapeutic mAbs in cell culture, measuring the neutralizing activity of the serum antibodies against either strain in recipients of either Ronapreve or Evusheld.
What Did the Study Show?
The antibodies tested for BA.2 neutralization included examples from all four classes of anti-RBD antibodies. Etesevimab (class 1) and Bamlanivimab (Class 2) were found in an early cocktail from Eli Lilly but are now obsolete in clinical practice. Regdanvimab (class 1), Sotrovimab and Adintrevimab were also included, apart from the four found in Ronapreve and Evusheld.
Seven of these proved ineffective against BA.2, the exceptions being Imdevimab and Cilgavimab. The IC50 of these were ~700 and 9 ng/mL, respectively, against BA.2, which is suggestive of better efficacy against this sublineage compared to BA.1. No further enhancement of efficacy was observed with the addition of Tixagevimab, as in Evusheld.
The scientists also found that immunocompromised people, most of whom were on anti-CD20 and prednisone for conditions like rheumatoid arthritis and kidney transplantation, responded well to Evusheld. Of the 29 patients in the study, 18 had been first treated with Ronapreve, and almost all had received three doses of the messenger ribonucleic acid (mRNA) SARS-CoV-2 vaccine BNT162b2 from Pfizer/BioNTech. Six had received four doses.
All received Evusheld PrEP because they had sub-threshold binding antibody levels after vaccination. Anti-spike immunoglobulin G (IgG) levels spiked from 5-60 binding antibody unit (BAU)/mL before treatment to 200-1300 BAU/mL afterward. Notably, those who had Ronapreve previously had anti-spike antibodies at ~800-1,000 BAU/mL when Evusheld was administered and showed no obvious response.
Thereafter, from day 3 onwards, stable antibody levels to the spike protein were maintained, or at most a slight increase.
The sera of these patients also showed no detectable neutralization activity on day 0, except for those who had received Ronapreve earlier. After Evusheld was given, neutralizing activity against the Delta variant increased steeply, to ~800-1,000 BAU/mL, while no increase was seen with those who had received Ronapreve already.
Ronapreve administration was not associated with BA.1 neutralization, but with Evusheld, 7/8 individuals acquired neutralizing ability against BA.1 over the period from day 3 to day 30. Nonetheless, the neutralizing titers were extremely low, not exceeding 130 BAU/mL at day 15, and some as low as 27 BAU/mL. An increase in neutralizing titers did occur from day 3 to day 15.
The mAbs appear to act poorly against BA.1 as indicated by the delayed neutralizing activity, at low levels, on day 3. No BA.2 neutralization was observed at day 0 in Ronapreve-naïve patients, and a low level of BA.2 neutralizing activity was seen after Ronapreve administration. This supports the earlier findings that Indevimab can neutralize the latter strain.
Evusheld administration was associated with an increase in BA.2 administration, with the 50% effective dose (ED50) going up to 3,500 on day 15. In most patients, neutralizing activity was maintained at stable levels, indicating that Evusheld has a long half-life.
Anti-spike IgG levels and anti-Delta neutralizing activity showed strong correlations, but not with anti-BA.1 or anti-BA.2 neutralization, indicating that Omicron has strong immune evasion capabilities.
What Are the Implications?
The results show that therapeutic mAbs vary significantly in their ability to confer neutralizing immunity against Delta vs Omicron, as well as Omicron BA.1 vs BA.2. In addition, untreated immunocompromised individuals reacted poorly to the vaccine, neutralizing neither Delta or either Omicron strain.
With Ronapreve, Delta was neutralized, but not BA.1, while neutralizing titers were low against BA.2. Evusheld led to detectable neutralizing activity against BA.1 in individuals who had not received Ronapreve, and 100% BA.2 neutralization, indicating that this cocktail neutralizes BA.2 better than BA.1.
The ED50 against Delta was >15,000 after Evusheld, and >70,000 after Ronapreve/Evusheld, but <50 against BA.1. Against BA.2, ED50 was above 1,500, indicating efficient neutralization even though the titers were reduced almost 10- and 40-fold compared to Delta neutralization. That is, neutralizing titers were comparable irrespective of whether both or only one mAb cocktail was administered.
“Our results support the importance of genomic surveillance.”
In order to protect against infection before exposure to the virus, the mAbs used must be active against the circulating variants. In the current situation, where BA.1 and BA.2 are co-circulating, mAbs like Bebtelovimab must be preferred, with activity against both strains.
Secondly, serologic tests that measure antibody binding and neutralization using the wildtype spike are misleading as they do not indicate protection against current strains.
“Future work will help determining whether adapted, lineage-specific, serological or neutralization assays can be used as a marker of clinical efficacy.”
As of now, treatment failures may be expected to become more frequent with the use of currently available mAbs, while the accumulation of more mutations will lead to the emergence of still more antibody-resistant strains. The use of either Ronapreve or Evusheld may be fraught with the risk of promoting the emergence of such escape mutations due to their low to intermediate neutralizing activity.
“We, therefore, recommend a close follow-up of these patients, particularly in case of prolonged infection despite treatment.”
- Bruel, T. et al. (2022). Serum Neutralization Of SARS-Cov-2 Omicron Sublineages BA.1 And BA.2 In Patients Receiving Monoclonal Antibodies. Nature Medicine. DOIhttps://doi.org/10.1038/s41591-022-01792-5. https://www.nature.com/articles/s41591-022-01792-5
Posted in: Medical Research News | Disease/Infection News | Pharmaceutical News
Tags: Antibodies, Antibody, Arthritis, Cell, Cell Culture, Coronavirus, Coronavirus Disease COVID-19, Efficacy, Genomic, immunity, Immunoglobulin, Kidney, Medicine, Omicron, Prednisone, Pre-Exposure Prophylaxis, Prophylaxis, Protein, Receptor, Research, Respiratory, Rheumatoid Arthritis, Ribonucleic Acid, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Sotrovimab, Spike Protein, Syndrome, Vaccine, Virus

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article
